The adaptive immune system is a highly specialised defense mechanism that protects the body against pathogens by recognising specific antigens and developing long-term immunity. Unlike the innate immune system, which responds rapidly but non-specifically, the adaptive system is slower on first exposure but produces a specific response and, most importantly, has immunological memory. This feature is key to how vaccinations work.
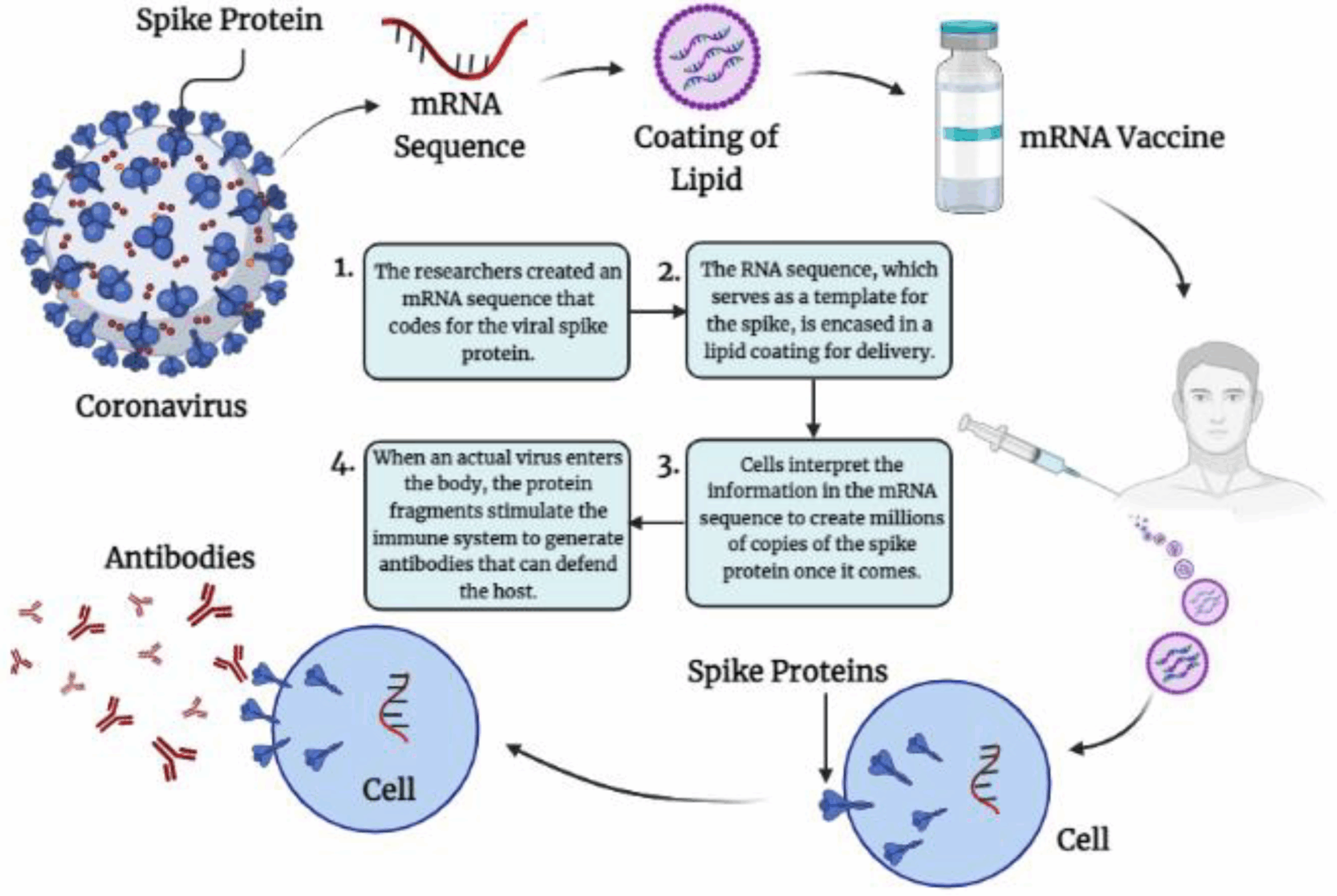
When a vaccine is introduced into the body, it contains either weakened, inactivated, or non-infectious components of a pathogen, such as proteins or inactivated toxins. These act as antigens that trigger the adaptive immune response without causing illness. B lymphocytes are activated and differentiate into plasma cells, which secrete antibodies that specifically bind to the introduced antigen. At the same time, some B cells become memory B cells, which persist in the body for years. Similarly, helper T cells activate both B cells and cytotoxic T cells, while cytotoxic T cells target and destroy any cells displaying the antigen. Memory T cells also remain in circulation after vaccination.
The first exposure through vaccination mimics the primary immune response, which is relatively slow and produces a moderate level of antibodies. However, the generation of memory cells ensures that, upon later exposure to the actual pathogen, the body can mount a secondary immune response. This response is rapid, producing a larger quantity of highly specific antibodies and activated T cells, often neutralising the pathogen before symptoms appear.
Vaccinations therefore harness the adaptive immune system’s specificity and memory, training the body to recognise and fight disease without the risks of natural infection. This principle not only protects individuals but also contributes to herd immunity, reducing disease spread within the community.
Chris Mylonas

